Rensselaer, NY – Neural Stem Cell Institute Scientists Advance Dementia Research Using 3D Brain Organoid Technology
Patients with dementia suffer from tau protein aggregation and brain degeneration especially in the cerebral cortex, the major brain region responsible for decision-making, memory, thinking, and normal interactions with family and friends. Tau protein aggregation occurs in brains of patients with Alzheimer’s Disease and of patients with rare genetic changes in the tau protein, which lead to early onset Frontotemporal Dementia (FTD); these and other related brain diseases such as Progressive Supranuclear Palsy (PSP) are known as ‘tauopathies’. Research led by Dr. Sally Temple, Scientific Director of the Neural Stem Cell Institute (NSCI), Rensselaer NY and Dr. Alison Goate, Director, Ronald M. Loeb Center for Alzheimer’s Disease at Mount Sinai, New York, N.Y, used stem cells derived from patients with tau mutations to study why brain cells die in tauopathies. This landmark study published in the journal Cell describes new insights into the dementia disease process and identifies candidate therapeutic agents to prevent disease progression.
“Patients who are diagnosed with dementia have typically already lost many brain cells in the cerebral cortex, the so-called excitatory neurons. The question we need to ask is what are the changes that caused these brain cells to die? If we knew the answer to that question, we could determine how to prevent brain cell degeneration and slow or prevent dementia progression”, said Dr. Temple.
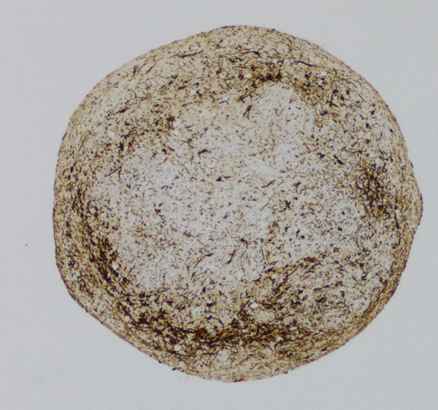
The research team used the new technology of creating brain organoids, small 3D models of living cells in the culture dish, some with the tau V337M mutation and some without this mutation for comparison. They discovered that these tau mutation ‘disease in a dish’ models, each about the size of a grain of rice, remarkably showed signs of tauopathy seen in patients with dementia, including tau accumulation and eventual death of the same excitatory types of neurons that are lost in patient brains.
Scientists at the Neuracell facility of NSCI created thousands of these brain organoids and worked with research teams at Mt. Sinai, NY, Washington University in St. Louis, MO, Massachusetts General Hospital, Boston, MA, and the University of Southern California (USC), Los Angeles, CA, to study how they develop signs of disease over time. The scientists discovered that tau mutation organoids show many early molecular changes prior to cell death. Notably, they also showed that they could prevent the death of these neurons by treating the organoids with an experimental drug or by genetic targeting of the altered pathways.
“Frontotemporal dementia is a devastating disease for patients and their loved ones. Understanding the causes of dementia can be difficult as most of the damage to the brain occurs well before any symptoms appear. It’s like trying to unravel the event that created a crime scene. In this study, we were able to model many aspects of the pathology seen in the brains of patients who carry the V337M mutation in tau,” said Alison M. Goate, DPhil., “Our results identified several very early transcriptomic and proteomic changes that lead to the formation of tau pathology and neuronal death. Our goal is to help researchers develop novel treatments against frontotemporal dementias and prevent the suffering experienced by patients and their families.”
Kathryn Bowles, Ph.D., an instructor in Dr. Goate’s lab at Mount Sinai, NY, led the study that documented the changes leading to cerebral cortex cell death in the organoids. “Excitatory neuron cell death, tau protein deposits, and inflammation are classic hallmarks of the kind of damage seen in many forms of frontotemporal dementia,” said Dr. Bowles. “What we wanted to know next was: what are the cellular and molecular processes that led to the appearance of these disease hallmarks? Our results suggest that the V337M mutant tau sets off a vicious cycle in the brain that puts excitatory neurons under great stress. It hastens the production of new proteins needed for maturation but prevents disposal of the proteins that are being replaced”.
Dr. Justin Ichida, John Douglas French Alzheimer’s Foundation Endowed Professor in Stem Cell Biology and Regenerative Medicine at USC then led studies that demonstrated the mutant organoid cells were vulnerable to stress caused by high levels of glutamate. They further found that this could be prevented by applying an experimental drug, apilimod, that is thought to alter how the cell recycles proteins from the cell surface membranes. While this research is in early stages, it suggests that patients with FTD and related dementias may early on have impaired glutamate signaling in the brain, and that correcting these impairments in time could rescue the cells from dying. This is certainly an important avenue of research going forward.
“This study shows the promise of stem cells to model and understand diseases like FTD and Alzheimer’s Disease and, most importantly, to illuminate new ways to combat these currently incurable diseases that afflict so many families,” said Dr. Temple.
This study was funded by the Rainwater Charitable Foundation, the National Institutes of Health (AG046374, AG054008, AG056293, NS110890, NS095252, NS097277, NS097850, NS117075), CurePSP, MGH Research Scholars Program, Association for Frontotemporal Degeneration, BrightFocus Foundation, Farrell Family Alzheimer’s Disease Research Fund, United States Department of Defense (W81XWH-21-1-0168, -20-1-0424, -21-1-0131), the Harrington Discovery Institute, CIRM, ALS Association, John Douglas French Alzheimer’s Foundation, ADDF, New York Stem Cell Foundation, and the Amgen Postdoctoral Fellowship.
Article information:
Bowles, K.R. et al., ELAVL4, splicing and glutamatergic dysfunction precede neuron loss in MAPT-mutation cerebral organoids. Cell, July 26, 2021 DOI: https://doi.org/10.1016/j.cell.2021.07.003

Leave a Reply